3D Printing Pioneer – A Decade in the Making
While scanning patients to create digital models of their limbs and 3D printing prosthetics might seem futuristic to some, South Beach O&P has been using this method successfully for years.
During a recent industry webinar, Tom Mills of South Beach O&P was interviewed by Aaron Naft of Comb O&P, focusing on South Beach and their adoption of digital.
The interview enlightened viewers as to how they could integrate digital workflows to accelerate device delivery while enhancing their patient care and how it is delivered.
Read the full transcript from Comb below.
How are you currently using scanning in your practice (how often, for which devices, etc.)?
We use scanning for all types of prosthetics. AKs, BKs, Upper Extremities, AFOs, KFOs, braces and orthotics. We also scan our models for digital storage. So, instead of taking up space with shelves of plaster and foam models, they are all stored on a local PC drive that we can access later if and when necessary.
What tools are you using for scanning, modification, and fabrication? Are you outsourcing fabrication?
For scanning, we use two devices to capture a model of the limb.
The first device is for fiberglass or plaster casts of the limb, which, traditionally would be filled with plaster then hand modified. Instead of filling the cast, we use the MedicoSoft DigiScan which is an upright device with a rotating laser and digital camera which captures the shape of the limb from the interior of a Cast.
The second device is the COMB app which we use to scan the limb directly. This has made it possible to bypass the casting and plaster filling stage in many cases and go straight to digital modification.
Now for modification, we have two 3D environment CAD programs that we use for digital modification. The primary software we use is MedicoSoft which is a robust 3D environment CAD software created by MEDICO for O&P.
The other software is Rapid Plaster, made by PVA, which we use for the final touches to our 3D print models prior to rendering.
As far as fabrication goes, we do everything in-house. We have a variety of machines and processes to create everything here.
We have the traditional cast and plaster fill method. We have two carving machines from Medico to carve foam models for Check Sockets & Lamination.
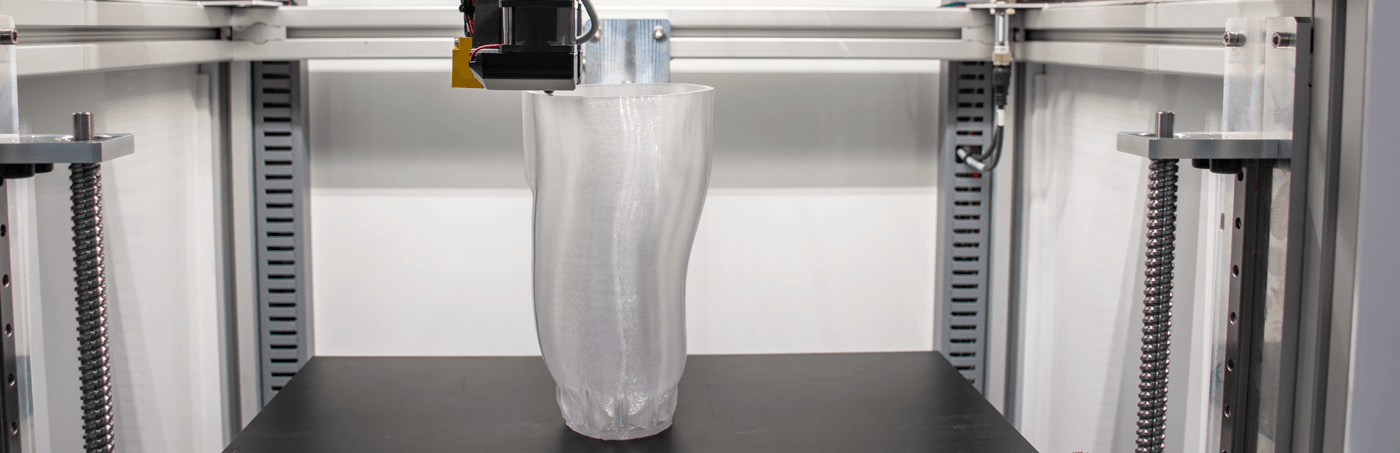
We have five Create 1400 3D printer machines for 3D printed BK check sockets. We have two Emergence Pro 3D printers from PVA for AK & BK check sockets. We have eight FLSUN 3D printers for making durable PLA covers for the limbs. And the most recent addition, we have a Precision 350 3D filament maker from 3DEVO to produce the PETG & PLA filament we use in all our 3D printers.
We recycle old check sockets and the waste VIVAK cutoffs to make regrind PETG that we put into the 3DEVO to produce the 3D filament. This reduces our environmental footprint and generates savings on the overall material cost to make check sockets.
How did you decide to make the move to digital? What was your decision process like?
Mark Selleck, the owner of South Beach has been moving into the digital frontier of limb fabrication for about a decade. Usually, a CEO’s choice is based on a company’s bottom line. It has been my experience that Mark is committed to excellence, accuracy, turnaround time, and improving the quality of life for his patients.
Our practice has a team of practitioners and reps that go directly to the patient. We see them in the hospital, hospice care, retirement facilities, and even to the patient’s homes. As such, a digital solution that can be mobile, “on-the-go” so to speak, was a natural evolution that fit for us.
Where is the value for you in digital? Is it costs, time savings, etc.?
You know, it is difficult to quantify the value of digital when there are so many factors to look at: cost, accuracy, quality, turnaround, etc. Looking at the savings from overhead, material, and labor costs alone are significant. The accuracy we get from digital is a major factor in saving costs.
Standard insurance allows two check sockets and one finished limb to be billed every two years; everything else is at a loss for the practice. With digital, we get the accuracy to fit the patient the first go around, thus eliminating additional time and material cost.
Digital supports pro-bono work as well. Then, there is the turnaround time to consider. Instead of the standard 1-2 months, the patient gets their finished limb in 1-2 weeks. Billing can be done sooner, the practice gets paid faster.
On a rush order, we can scan the limb, digitally modify it, carve a foam model, pull Vivak, and check the fit all in one hour. The CS can then go to LAM for the finished form and deliver the limb to the patient by end of the week.
A big factor is the quality of life for the patient. Speaking for myself, I am an RBK amputee. For 15 years, I have worn a lot of limbs made from all the traditional fabrication methods from six different prosthetic companies. Every single one has caused me pain and discomfort, some more than others. I would tailor my life around the limb and its capabilities, weighing the cost/benefits of how much pain and recovery would I be willing to endure to accomplish the task or undertake the adventure. A surprising number of amputees like myself just deal with it; “At least this one doesn’t hurt me as much as that other one.”
The current leg I am wearing came from a digital scan about two years ago and for the first time since I lost my leg, I have been able to move about in comfort to the point that there are days I forget I am wearing a prosthetic.
Do you believe that the digital workflow will be more widely used in O&P over the next few years? If so, why?
Absolutely. More and more digital options are being made available and cost-effective that produce a consistent, reliable product. There are even designs available online that amateurs can access and print at home DIY style.
I believe the major hurdles in the way have been the exorbitant cost of going digital and the learning curve required to integrate a digital method. Not to mention, all the products and items that simply do not work that are being marketed today. I imagine it is hard for a small practice to take the leap of faith for that type of investment when they know little about it or even where to begin.
That being said, digital is the obvious choice to transcend current traditional methods of fabrication.
What advice would you give to the thousands of practitioners around the world exploring digital for the first time?
First and foremost, digital is not a cookie-cutter, one size fits all. Each practice is unique and what works for one may not fit your business model. Do not settle for a solution. Be patient and take your time choosing what will work best for your practice. The solution should fit your practice, not the other way around.
Do plenty of research. Speak to the big player in O&P using digital like Open Bionics, Nia Technologies, Comb, PVA Med, Medico, e-NABLE, WillowWood, etc., and don’t be afraid to ask them to recommend other people and companies that do what they do so you can expand your research.
Hire an IT savvy person to do some of the heavy lifting on research and overcome the learning curve and then have them teach it to you and your staff.
Be a visionary and see how this will transcend the traditional and open a new world of possibilities for your practice and improve upon the quality of life for the patients you care for.